Stack 2006-2007
Ophthalmology Questions
Question
1.
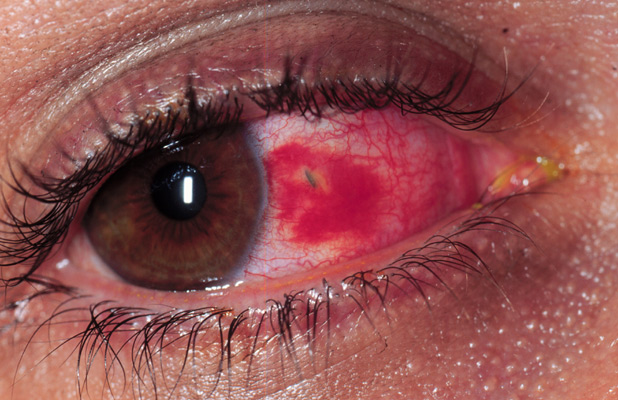
A 23 year-old male presents to the emergency department complaining of eye pain after a foreign body fell from his car while fixing a muffler. Visual acuity is 20/30 in the affected eye. His eye is seen here.
Which of the following is the next best test to evaluate this patient?
- MRI
- Intraocular pressure with a Tonopen
- CT scan of the orbits
- Ocular ultrasound
- Plain films of the orbits
Correct answer is C.
This patient has an embedded foreign body of the sclera. A surrounding subconjunctival hemorrhage is also present and is of no consequence. Determination of the size of the foreign body and its degree of penetration is important issue for this patient. This foreign body seems to have a metallic texture and therefore and MRI would not be a good choice for evaluation of this injury. Metallic fragments may be moved by the magnetic field of the MRI scanner and potentially cause more damage to the globe. Since an open globe is a possibility, avoid tests that may extrude intraocular contents. Therefore tonometry and ocular ultrasound should be considered only if there is no other option. Plain films may detect the presence of a metallic foreign body within the orbit, but will not allow discernment of the weather the globe as been penetrated or not. CT scan of the orbits allows a 3-dimensional evaluation of an ocular foreign body and is the best test to evaluate this injury. Globe collapse, retinal detachment, vitreous bleeding may be seen on CT scan.

The metallic foreign body is seen at the level of the nasal aspect of the sclera. It does not appear to have penetrated the vitreous. The globe seems normal contour and does not appear collapsed. Ophthalmology was consulted for removal of the foreign body.
Question
2.
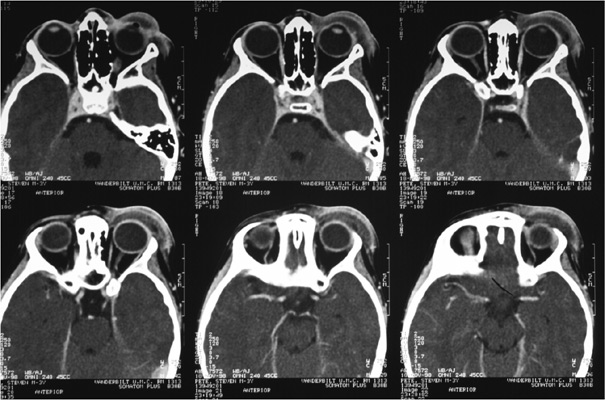
A 3 year-old male presents to the emergency department with fever, pain, and swelling of the left periorbital tissues as seen below. He is currently taking amoxicillin/clavulanate for a dog bite he suffered to his face 3 days prior. He appears ill and will not allow you to open his eyelid due to pain. Review of the initial ED visit for the bite shows the globe examination was normal. A contrasted CT scan of the orbits is shown below.

Which of the following is true regarding this case?
A. Orbital cellulitis seen here should be treated with operative decompression of the orbit.
B. Preseptal cellulitis seen here should be treated with intravenous antibiotics to cover Staphylococcus species, Streptococcus species, and Pasturella multicida.
C. Open globe seen here warrants an ophthalmology consult.
D. The subarachnoid hemorrhage seen here warrants a neurosurgery consult.
Correct answer is B.
This patient as preseptal (periortibal) cellulitis
Question
3.
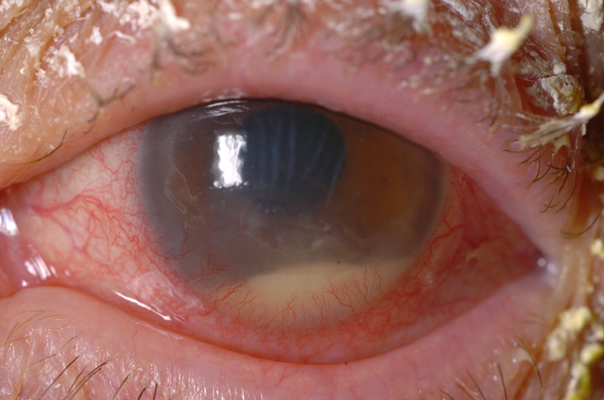
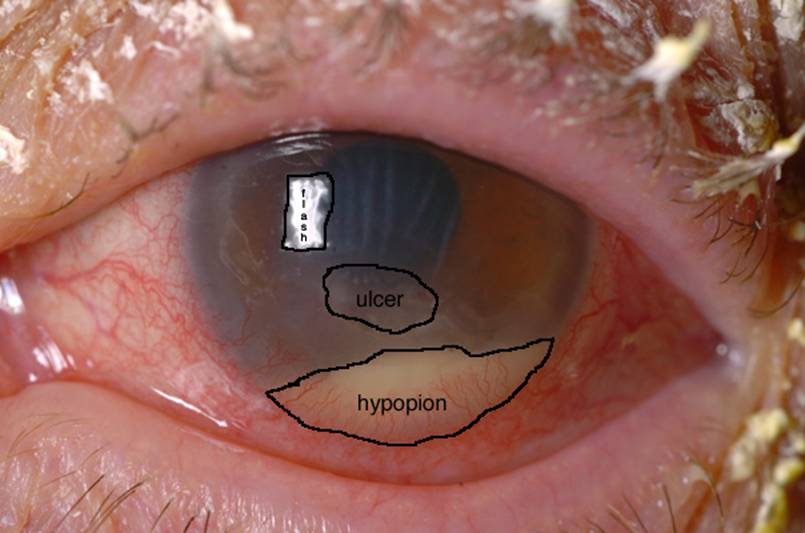
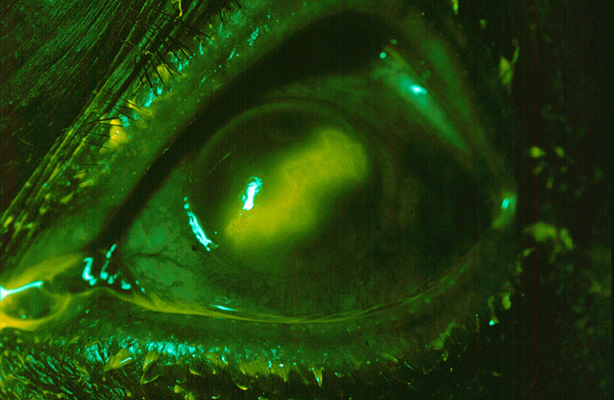
An 85 year-old female comes to the emergency department because of decreased vision, a foreign body sensation, and left eye pain for 3 days. Symptoms started gradually without history of any trauma. This patient has a history of posterior intraocular lens implant and dry eyes. Visual acuity of the left eye is hand motion only at 2 feet. Extraocular movements are normal. Pupils are 3mm round and reactive to light. Intraocular pressure is 22 mmHg in the left eye. Fundus was not visualized.
The external examination is seen below:
Management of this condition includes all of the following except:
- Hospitalization for frequent (q1h or less) administration of broad spectrum topical antibiotics
- Ophthalmology consultation
- Culture and gram stain of the corneal surface
- Immediate anterior chamber paracentesis
Correct answer is D.
This patient has a corneal ulcer, seen at
Question
4.
This 70 year-old female presents to the emergency department
at
Emergency department treatment of this patient may include all of the following except:
- Topical steroids
- Topical antiviral drops
- Oral acyclovir
- Close outpatient follow-up
- Ophthalmology consultation
Correct answer is A
This patient has herpes simplex keratitis (HSK). Symptoms of HSK include eye pain, redness, tearing, decreased vision, and photophobia. Corneal vesicles coalesce into a dendritic pattern as seen in the photograph above. Treatment of this condition is topical antiviral drops such as trifluridine 1% or vidarabine 3%. Topical antiviral agents cause corneal toxicity and should be tapered in 2-3 days which is the time when clinical improvement is usually seen. Oral antiviral agents such as acyclovir are effective and does not result in corneal toxicity.
Question 5.
A 53 year-old male presents to the emergency department at 2AM with swelling and pruritis of his right eye. The day before he removed a tiny bug from his eye which he encountered while riding his motorcycle. He denies any pain. His visual acuity is 20/40 in the affected eye. Fluorescein stain of the cornea is normal. Funduscopic examination is normal. Extraocular movements are normal. Intraocular pressure is normal. External findings are shown below:

Which of the following is the correct treatment of this patient’s condition?
- Ophthalmologic topical antihistamine Vasocon-A (naphazoline hydrochloride, antazoline phosphate)
- Cool compresses
- Irrigation of the eye
- All of the above
Correct answer is D.
This patient has allergic conjunctivitis with moderate chemosis (edema of the bulbar conjunctiva). This is most likely due to insect protein allergy based on his history. Symptoms of allergic conjunctivitis include pruirits, gritty foreign body sensation, and watery discharge and typically involves both eyes. The pale edema of the conjunctiva is characteristic of allergic chemosis. Treatment of this patient includes irrigation of the eye to remove bug remnants, topical decongestant-antihistamine combination drops, and cool compresses. Ophthalmology consultation is usually not needed.